Abstract
Background: Eltrombopag or Romiplostimare the two thrombopoietin mimetics that have been FDA-approved for the treatment of ITP in patients with an insufficient response to corticosteroids and intravenous immune globulin. However, there are no studies comparing in the real world setting the benefits and risks of these treatments.
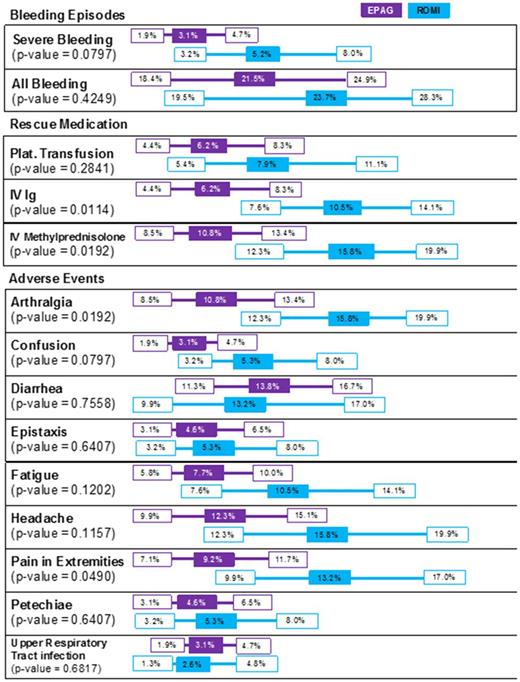
Aims: To compare benefits - bleeding related events (BREs) and use of rescue medication (RM), and risks - adverse events (AEs), in patients with ITP treated with EPAG or ROMI.
Methods: This study used a syndicated electronic medical records network containing information on inpatient/outpatient services and procedures, diagnoses, prescribed medications, and labs for over 29 million patients from 26 US hospital institutions. Adult patients diagnosed with primary ITP (ICD-10 D69.3) and treated with EPAG or ROMI were similar in age, prior steroid treatment, history of HBV/HCV/HIV, severe aplastic anemia, myelodysplastic syndrome, myelofibrosis, other malignancies and splenectomy. Incidence proportion of patients who experienced BREs, RM use, platelet transfusions, and AEs (based on a list of diagnostic codes) were calculated over the 12 months following treatment initiation. Severe BREs were defined as BRE requiring platelet transfusions. Relevant AEs were selected based on FDA prescribing information for EPAG and ROMI. Incidence proportions of patients with each outcome and their 95% confidence intervals (CIs) were descriptively compared for each outcome using Z-tests with two-tailed α=0.05.
Results: Among 1070 identified ITP patients (EPAG 680, ROMI 390) mean age was 60 years (SD: 18) and 51% were male. Incidence proportions of patients with all BREs, severe BREs, RM (IVIG and IV methylprednisolone) use, and AEs (arthralgia, confusion, epistaxis, fatigue, headache, pain in extremities and petechiae) were lower in EPAG patients, while the incidence proportions of patients with diarrhea and upper respiratory tract infections were lower in ROMI patients. Statistically significantly lower rates were only observed in patients on EPAG for: lower RM (IVIG and IV methylprednisolone) use, arthralgia and pain in extremities (See Chart).
Conclusions: This is the first comparison of benefits and risks in patients with ITP treated with EPAG or ROMI that suggests a potential advantages of the EPAG use, especially the lower rates of RM use. Study limitations include biases associated with reliance on outcomes reporting in hospital records with potential missing data, limited longitudinal data and biases related to indirect treatment comparisons based on real world data.
CHART: Benefit-Risk Comparison in ITP (% of patients with events over 12 months).
Roy: Novartis: Employment, Equity Ownership. Bhor: Novartis: Employment, Equity Ownership, Research Funding. Allepuz: Novartis: Employment. Portella: Novartis: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal